Attention primary care physicians: You or your clinical staff may be treating a select patient population and leaving untapped revenue on the table.
Every business leader knows that time equals money. So, when physicians don’t bill for patient work performed outside the clinical setting, time ceases to be about income and instead becomes a symptom of an issue every business dreads: missed revenue.
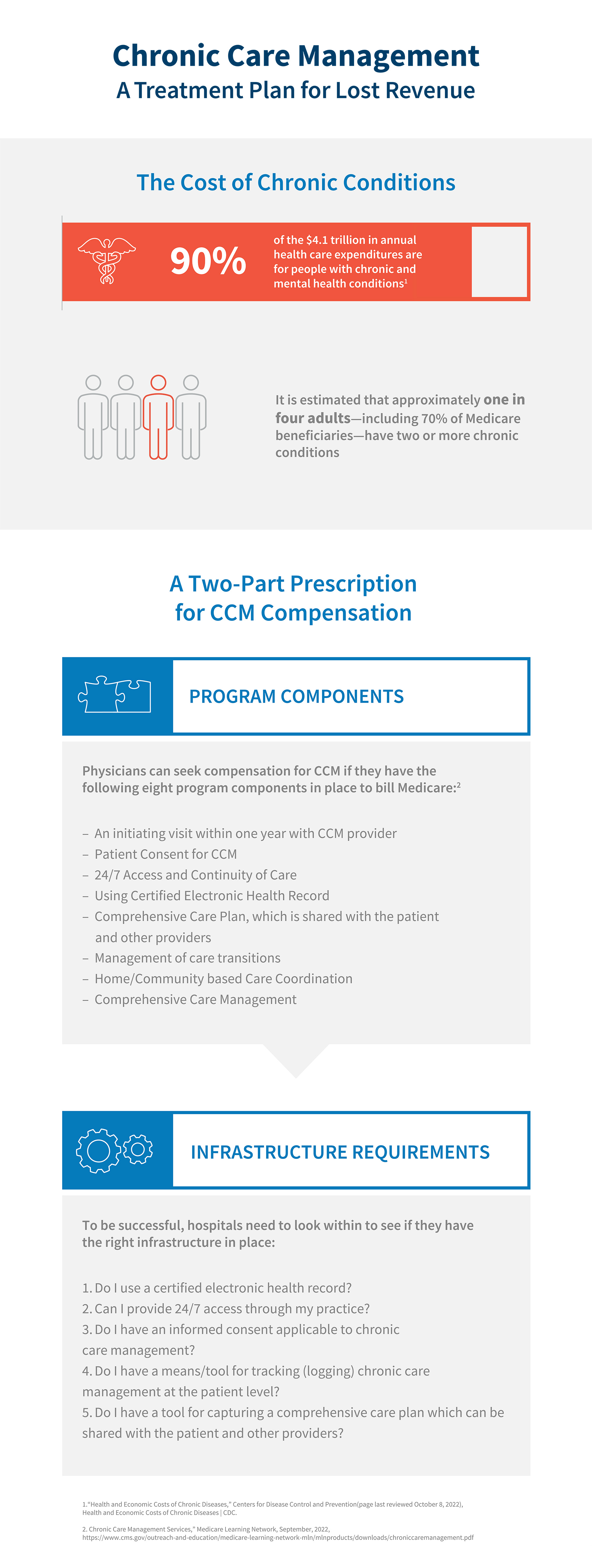
There’s a remedy for that. Chronic care management (“CCM”) is a reimbursable service designed to compensate medical providers and their clinical staff for time spent outside of traditional evaluation and management visits.1 The potential is enormous considering that 90% of the $4.1 trillion in annual healthcare expenditures in the United States is attributed to patients with chronic and mental health conditions.2
Medical providers are all too familiar with the heavy lifting that goes on behind the scenes with patient care. They devote vast amounts of time emailing, calling and sending paperwork to other providers involved in caring for the patient. They manage the transition of the patient’s care to at-home or community-based services and ensure the patient has access to other qualified healthcare professionals.
Like the managed care movement, the goal of CCM is to support patients’ primary care and empower individuals to use self-care management with the assistance of a provider.3 Meanwhile, many providers are either unfamiliar with CCM or they avoid it for reasons outlined below. That’s unfortunate, because in addition to leaving revenue on the table, they’re missing out on the opportunity to bring in new patients looking for coordinated care.
CCM Reimbursements
Both the Medicare Physician Fee Schedule (“MPFS”) and the Outpatient Prospective Payment System (“OPPS”) cover CCM services. The 2022 MPFS reimburses physicians an average of $60 for a minimum of 20 minutes spent on a patient per month, and $116 for a minimum of 60 minutes of Complex CCM time.4 In 2022, OPPS has paid hospitals $76 for a minimum of 20 minutes per month and $137 for a 60-minute minimum.5
What is scaring off physicians from using CCM? For starters, the coding for different services can be onerous. On top of that, there are several requirements — such as having certified electronic healthcare records — that put physicians in a position where they need to make further investments to reap the benefits of the system. For example, many hospitals have adopted electronic healthcare records, but not all private practices have done the same.6
There’s no doubt that many providers deliver chronic care services and deserve to be compensated for the time they spent caring for patients. However, navigating the complex landscape of tiered codes, billable hours and regulations can be a daunting task. Below are a few insights that hospitals and physicians should consider if they want to find success with a CCM program.

For further information, please contact:
Nancy L. Freeman, Managing Director, FTI Consulting
nancy.freeman@fticonsulting.com
1: “Chronic Care Management,” American Association for Family Physicians (page last reviewed October 6, 2022), https://www.aafp.org/family-physician/practice-and-career/getting-paid/coding/chronic-care-management.html
2: “Health and Economic Costs of Chronic Diseases,” Centers for Disease Control and Prevention (page last reviewed October 8, 2022), https://www.cdc.gov/chronicdisease/about/costs/index.htm.
3: Chronic Care Management Services,” Medicare Learning Network, September, 2022, https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/chroniccaremanagement.pdf
4: “Search the Physician Fee Schedule,” Centers for Medicare & Medicaid Services (page last reviewed on October 8, 2022), https://www.cms.gov/medicare/physician-fee-schedule/search
5: “License for Use of Current Procedural Terminology, Fourth Edition (“CPT®”), Centers for Medicare & Medicaid Services (page last reviewed on October 8, 2022), https://www.cms.gov/license/ama?file=/files/zip/addendum-b-july-2022.zip
6: “Private practice physicians less likely to maintain electronic records, study shows,” Healthcare Finance, July 22, 2019, https://www.healthcarefinancenews.com/news/private-practice-physicians-less-likely-maintain-electronic-records-study-shows





