As companies weigh their options for bringing employees back to the office, the physical and mental health of their people should be a top priority — for their sake, and for the economic health of our communities.
The massive economic and social disruption of the pandemic has led to a dramatic rise in stress and health issues for many of us. But that may be just the tip of the iceberg when it comes to the impact of the pandemic on our well-being. Longer term, we can expect to see many people, especially those with chronic conditions, continue to need additional care and support as a direct result of COVID-19.
Medical experts, say the impact on the workforce, in particular, could be so profound that entire local economies will be affected, suppressing growth and resilience1. Indeed, pre-pandemic data collected by FTI Consulting’s Center for Healthcare Economics and Policy for two metropolitan areas, Buffalo and Nashville, portends trouble. Just three chronic conditions — diabetes, hypertension, and depression — cost the two areas $1.4 billion and $2.0 billion respectively, in annual lost productivity and medical expenditure. (The Buffalo figure represents over 2% of its regional GDP2.)
The issue is on the minds of employers as they prepare for the large-scale return of workers to the office. More than 1,000 employed professionals surveyed by FTI Consulting in September said the top business priority for CEOs should be the physical health and well-being of employees.
Civic leaders are concerned about the long-term economic and social consequences of the pandemic. More than half (52%) of respondents in a 2021 Boston University survey of U.S. mayors said they were worried about lingering mental health challenges and trauma.
With chronic conditions so pronounced among the U.S. public (see “Prevalence of Chronic Conditions” chart) it’s clear the issue cannot be ignored. Nor can it be tackled piecemeal or in silos. If we are to improve the health of such vulnerable populations and foster economic growth and resiliency, we will need strong cooperation among business, civic and community leaders, including public-private partnerships and collaboration with state and local health departments.
Doing so brings together trusted partners from across a community who can attract and organize the substantial financial resources needed from local, state, and federal levels for successful action3.
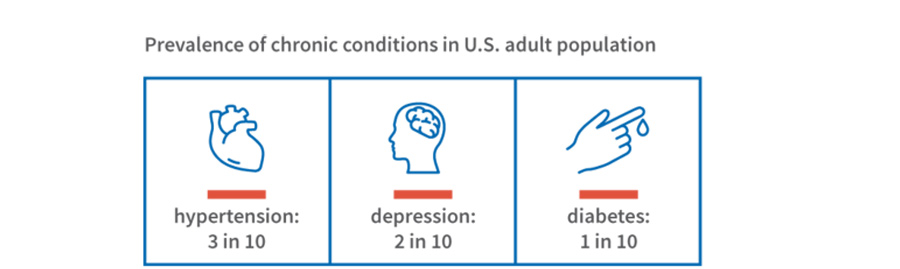
Source: Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Population Health, BRFSS Prevalence & Trend Data for 2020, accessed Jan 2022. High blood pressure data from 2019. Obesity prevalence is 3 out of 10. Prevalence rates vary across metro regions and states.
First Things First
Addressing chronic conditions within the workforce benefits all parties. Employees become healthier. Productivity rises. Cost savings follow through reduced medical utilization and spending, lower insurance costs, and improved employee retention.
Businesses and communities in turn realize greater opportunity for economic vitality. (In fact, productivity costs from chronic conditions often add unrecognized economic cost to those measured by spending on healthcare benefits alone — e.g., insurance and out-of-pocket costs.)
Some employers are a step ahead, having responded to employee needs by expanding coverage for mental health and telehealth, offering more personal time and paid sick leave, and incentivizing participation in wellness programs.
While these benefits are helpful, experts believe that more attention needs to be paid to mental health and deferred health on a public scale to improve the health of the workforce4. Health interventions that improve diagnosis, management and treatment of health conditions provide more access to care and prevent diseases from progressing to later stages offer substantial savings not just to businesses, but to their entire local communities.
Arriving at this new state will not be easy, as all parties know.
The Challenges
Business leaders face several challenges when it comes to effectively addressing employee health coming out of the pandemic. First, they are deluged with information about the pandemic’s impact and potential drivers of poor health, making it difficult to know which specific health issues to focus on for greatest returns. Further, they often lack the data on how specific chronic conditions affect their workforces and local communities, as well as the financial consequences of poor health. Perhaps most significantly, they are often uninformed about the most effective health interventions and the critical factors for success.
Another challenge stems from the pandemic’s disruption of care delivery, which has exacerbated chronic conditions in the public. The lockdown and the focus on treating COVID-19 patients has led many of us to defer healthcare visits — routine or otherwise — which leaves returning employees with chronic conditions in poorer health than before the pandemic5.
These challenges reinforce the need for cooperation among civic, government and business leaders about the potential benefits from innovative and effective investment in public health.
The Solutions
Though the scale of the issue may be daunting, the good news is that targeting just one or two chronic conditions — diabetes and hypertension, for example — can lead to dramatic results in the workforce and beyond. Both conditions are highly prevalent, accounting for a very large share of medical and productivity costs for many metro areas.
Two intervention programs, one in Cincinnati, Ohio, the other in Rochester, New York, demonstrate the efficacy.
Cincinnati: A major supermarket chain partnered with a large health insurer to use specially trained pharmacists to help both the city and their own employees manage hypertension. The number of employees with high blood pressure dropped from 48% to 30%, and medical costs for those employees were reduced by as much as $400 annually. The program also helped employees improve their management of diabetes.
Rochester: A blood pressure registry launched with support from business and local leaders provided guidance on blood pressure control. The result: 9 in 10 patients working with an advocate got their blood pressure under control, and the share of residents with high blood pressure dropped significantly over time.
Of course, interventions are not one-size-fits-all. Health needs, priorities, resources and leadership groups vary from region to region. But tailoring and scaling intervention programs is very much a viable approach.
Investing in People Is the Future
As the worst of the pandemic wanes, we enter new, uncharted waters. Calls for racial and social justice, and the “Great Resignation,” have changed workforce expectations. Today’s employees want their companies to place their health and well-being front and center.
Initiatives along those lines were taking shape prior to 2020, but a new perspective is needed. One in which business leaders look at healthcare not primarily as a cost of doing business, but as an investment in their people and the future of the business.Business leaders must look at healthcare not as a cost of doing business, but as an investment in their people and the future of the business.
Opportunities for action are wide-ranging. Targeted interventions of prevalent chronic conditions yield substantial benefits that can be scaled as needed. Innovative tools like healthcare dashboards that consolidate key current performance indicators and action items are starting to be deployed. In many communities, broader coalitions among business, civic and community leaders are already aligned to address the impact of the pandemic and are positioned to do more.
Bottom line, improving workforce health is in the best interest of us all. Helping reduce the risks of the pandemic and whatever may follow, while advancing growth and vitality for businesses, workers, and communities, lifts all boats.
Let’s seize the moment.

For further information, please contact:
Margaret E. Guerin-Calvert, FTI Consulting
margaret.guerin-calvert@fticonsulting.com





